
Why acoustics matter in elderly care
Age-related hearing loss (presbyacusis) causes communication problems for approximately 37% of people between the ages of 61 and 70. This prevalence rises to 60% for people aged 71 to 80(1).
More consultations for citizens + 80 years
From 2009 – 2014 (in Denmark), the only group of patients who consults a doctor more is the group of patients who are + 80 years old. All other age groups consult a doctor less. Citizens aged 80 or older represent 10% of all consultations – despite the fact that they make up only 4% of the population(2).
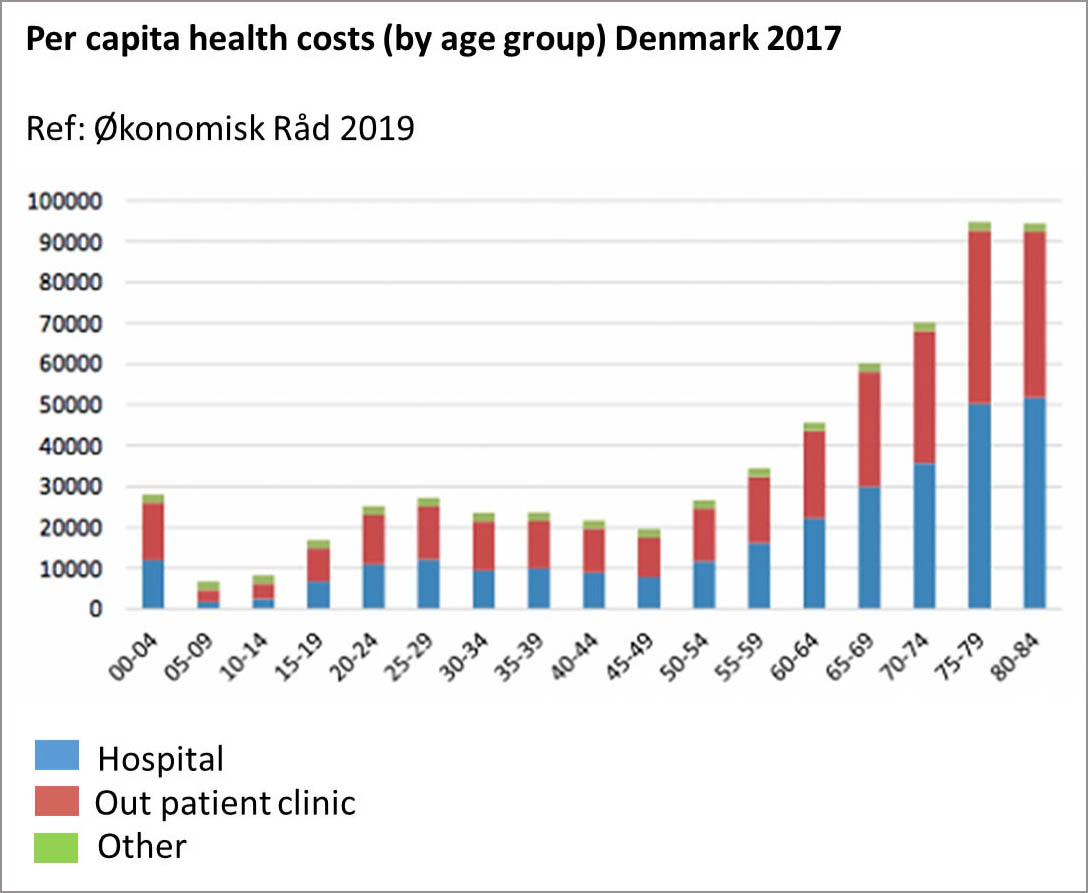 Furthermore, if we look into health costs we also see that citizens aged 75 and older top the list over age groups that have the highest health costs.
Furthermore, if we look into health costs we also see that citizens aged 75 and older top the list over age groups that have the highest health costs.
These numbers tell us that we have more and more ‘elderly ears’ in our healthcare facilities today than we used to and therefore we need to consider this fact when we build and refurbish rooms that should support communication, cure and care.
People who are cut off acoustically from the external world not only lose their hearing, they are at risk of becoming socially and intellectually isolated. The less stimulation the brain receives, the more quickly its capacity diminishes.
Intervention study in Århus, Denmark
In a dementia clinic in Denmark the building did not support the activities in the rooms – and it didn’t support the elderly ear. The rooms were all done with hard surfaces and no acoustic treatment were used. This caused a noisy sound environment with long reverberation times and bad speech clarity. Exactly what you don’t need in elderly care.
Collaboration with The Technical University of Denmark (DTU)
As part of his BA-project Rasmus Qupersimat Jørgensen from DTU investigated the clinic both in regards to room acoustics but also in regards to end-user satisfaction.
Rasmus conducted room acoustic measurements before and after installing an acoustic ceiling (see picture) in one of the offices/examination rooms and he handed out questionnaires to the staff. Furthermore, he did an in depth interview with one of the doctors to learn more about how the sound environment was affecting both staff and patients.
The examination room
The room used for the study is used for communication and cognitive testing of the patients on a daily basis. Often relatives participate together with the patient which means that there is more than one speaker at the time.
The examination room is approximately 16 m2 and all the surfaces are hard; the floor is wooden and the walls are concrete and gypsum. The ceiling is a sound reflective plasterboard solution. The intervention was to change the acoustically reflective ceiling to one which absorbs sound.
Because of fire demands and a low ceiling height it was not possible to make the best acoustic solution: a suspended ceiling in a grid system. To make sure that the clinic could still live up to the building regulation in regard to ceiling height and fire demands a glued 20 mm. solution was mounted (Ecophon FocusTM B).
Measurements and guidelines
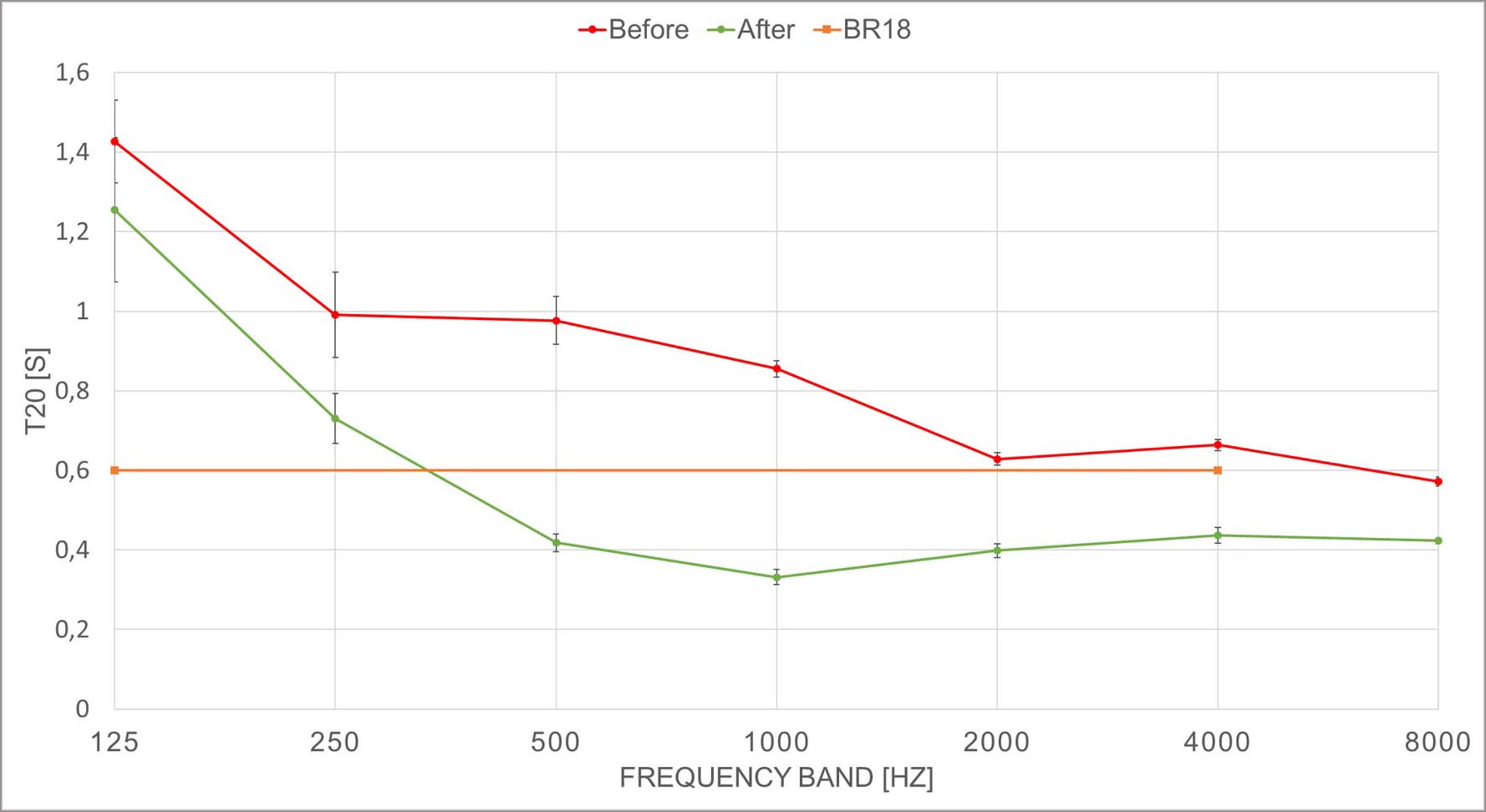
The before and after measurements in the clinic revealed that even though the acoustic treatment was a compromise, it made a big change. According to the Danish acoustic guidelines for healthcare examination rooms (BR19) one should reach reverberation time (T20) ≤ 0.6 seconds (with a variation of 20% for the 125 Hz) – and there is no doubt that just installing the ceiling makes the reverberation time drop to a much better level almost living up to the guideline. Before the treatment the guideline is not met on any frequency.
Speech clarity
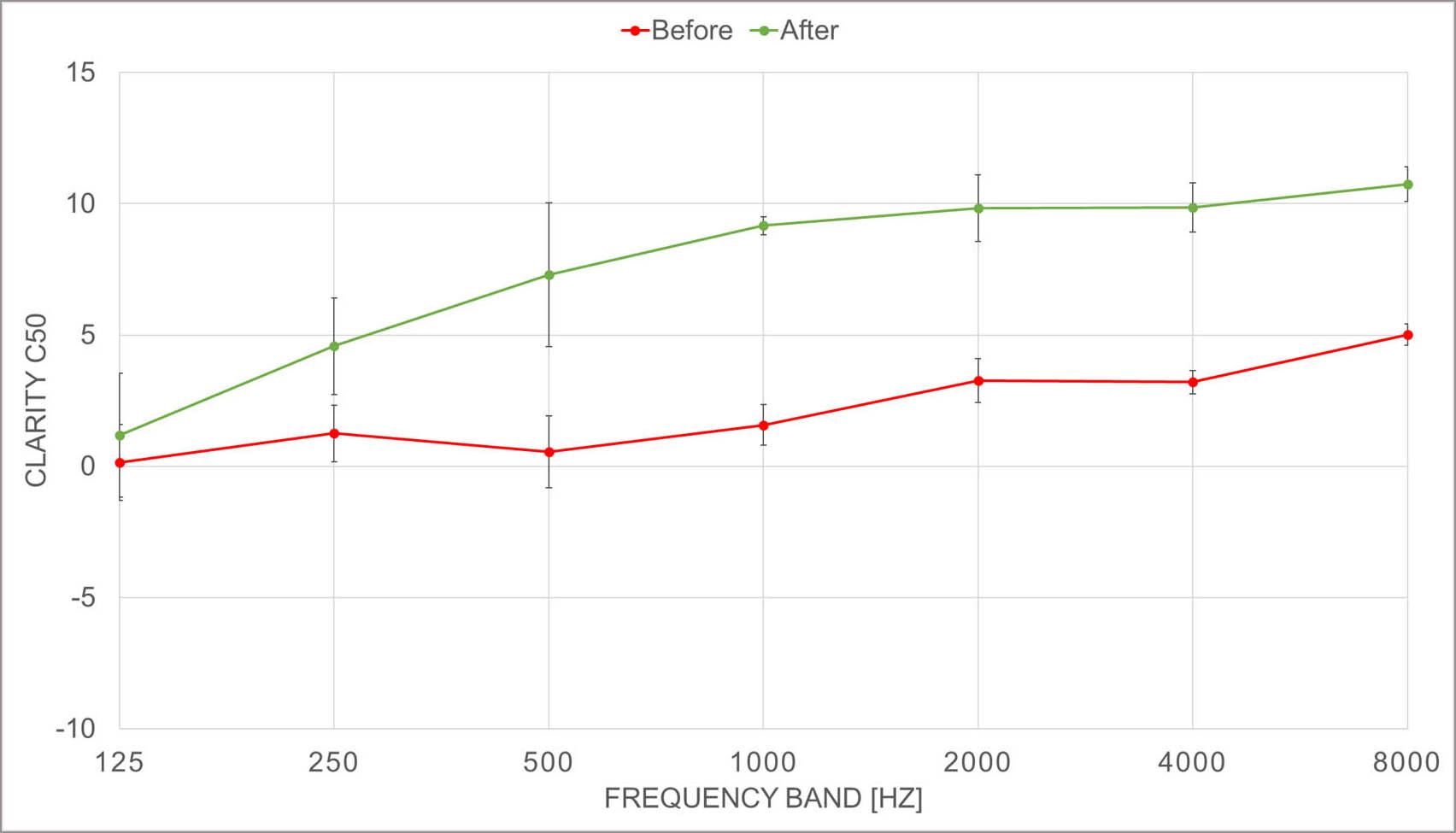
To support the elderly ear, it is important to also have good speech clarity in the facility and therefore C50 – clarity was also evaluated. Clarity is not yet in the Danish guideline but knowing that the just noticeable difference is 1 dB it was interesting to see, what impact the acoustic treatment had. Improvement on all frequencies were seen and from 350 Hz and up – there are more than 5 dB difference between before and after! On paper (!) this is a huge difference.
End-user statements
The doctors who took part in the project were all very positive about the room acoustic changes.
I could feel a big change. I no longer have to do the same effort in order to speak a certain way, the conversation is very relaxed now.
The in depth interview with one of the doctors revealed that before the acoustic treatment they were often in risk of making mistake during the cognitive testing. Sometimes a patient could have hearing impairment without ‘showing it’ – and then the doctor could be in doubt whether a wrong answer was because of bad hearing or cognitive deficits (because of dementia).
(1) Baur et al., Einfluss exogener Faktoren auf Altersschwerhörigkeit, HNO 2009, Springer Medizin Verlag 2009, p1023–1028.
(2) Momentum 2015
(3) Arneborg, E., Deutsche Seniorenliga e.V., Altersschwerhörigkeit – Symptome, Ursachen, Folgen, Diagnostik, Therapie, (Age-related hearing loss – symptoms, causes, consequences, diagnosis, therapy) Ausgabe 2010; Dalton et al., 2003; Chia et al., 2007; Chisolm et al., 2004
